Optimizing Eye Comfort and Managing Dry Eye
 Some patients observe awareness of dry eye symptoms, often in association with contact lens wear, or after laser vision correction care such as LASIK or PRK. There are several reasons why this might be the case, and they do not relate to the surgery in the overwhelming majority of instances. They relate more to our ability to help patients understand the numerous contributing factors to dry eye, and how to manage these in our warm, dry, desert climate. With all vision correction care we endeavor to optimize the ocular surface both before and after surgery, provide careful follow-up care, and attend to numerous details in the process.
Some patients observe awareness of dry eye symptoms, often in association with contact lens wear, or after laser vision correction care such as LASIK or PRK. There are several reasons why this might be the case, and they do not relate to the surgery in the overwhelming majority of instances. They relate more to our ability to help patients understand the numerous contributing factors to dry eye, and how to manage these in our warm, dry, desert climate. With all vision correction care we endeavor to optimize the ocular surface both before and after surgery, provide careful follow-up care, and attend to numerous details in the process.
 The normal cornea is very sensitive to touch, foreign body sensation, and mild superficial injury. Anyone who has ever had an eye infection, contact lens-related irritation or corneal scratch knows this to be true. A network of sensory nerves provides this exquisite sensitivity. If the ocular surface is chemically irritated (by exposure to noxious substances in or near the eye), or otherwise disturbed (mechanical injury, etc.), this can cause the eye or eyes to become irritated, red, and sore. All of these symptoms (irritation, redness, dryness, soreness, and sometimes excess tearing as a reflex to dryness) can be manifestations of ocular surface irritation. In LASIK, creation of the flap causes some of the sensory nerves to be cut, which actually diminishes sensitivity. I tell patients that it is ‘as if the phone lines are down;’ such that the eye surface cannot convey to the tear gland when additional moisture is needed. Typically, these nerves do grow back, and sensitivity returns to reasonably normal levels within about three months of treatment.
The normal cornea is very sensitive to touch, foreign body sensation, and mild superficial injury. Anyone who has ever had an eye infection, contact lens-related irritation or corneal scratch knows this to be true. A network of sensory nerves provides this exquisite sensitivity. If the ocular surface is chemically irritated (by exposure to noxious substances in or near the eye), or otherwise disturbed (mechanical injury, etc.), this can cause the eye or eyes to become irritated, red, and sore. All of these symptoms (irritation, redness, dryness, soreness, and sometimes excess tearing as a reflex to dryness) can be manifestations of ocular surface irritation. In LASIK, creation of the flap causes some of the sensory nerves to be cut, which actually diminishes sensitivity. I tell patients that it is ‘as if the phone lines are down;’ such that the eye surface cannot convey to the tear gland when additional moisture is needed. Typically, these nerves do grow back, and sensitivity returns to reasonably normal levels within about three months of treatment.
For this reason, we tell all patients that it is very important to use artificial tear eye drops on a very frequent basis for at least first 2 or 3 months after LASIK, and longer if desired to maintain or increase comfort. I advise use of tears as often as every couple of hours through the day, or whenever one remembers to put in a drop. If preservative-free tears are used, there is no hazard to over-use. There are many formulations and brands of artificial tears available. We like and currently recommend Thera-Tears, GenTeal, and Systane among others. If used in a reasonably diligent fashion for the recommended interval, dryness symptoms can be reduced to a manageable minimum, or eliminated.
Lubricant Gel can be a useful adjunct at night before retiring if necessary. We have used GenTeal Gel, Systane Gel and Thera-Tears Liqui-Gel with good success. These products are longer-lasting than eye drops, but the trade-off is that they are a bit too ‘goopy’ to be useful during the day, when eyes are open. There are several in-between products including Thera tears Liqui-Gel drops, GenTeal “Moderate to Severe” drops and others, which can be used during the day and do not impair visual function as much as the night-time gels.
 Climate and environment are very significant influences on eye comfort, and on tear requirements. Ambient temperature and humidity are critical factors. It is my experience that far fewer people complain about dry eyes in regions where the air is moist and cool (such as San Francisco, Seattle or Vancouver), compared to other regions where air quality is hot and dry (Palm Springs, San Bernardino, Bakersfield, Las Vegas, etc.).
Climate and environment are very significant influences on eye comfort, and on tear requirements. Ambient temperature and humidity are critical factors. It is my experience that far fewer people complain about dry eyes in regions where the air is moist and cool (such as San Francisco, Seattle or Vancouver), compared to other regions where air quality is hot and dry (Palm Springs, San Bernardino, Bakersfield, Las Vegas, etc.).
Southern California weather is often hot, dry, dusty and sometimes smoggy. When weather conditions include high pressure over the desert, our Santa Ana winds make for particularly warm, windy, dry conditions. Low humidity, wind, warm weather and poor air quality clearly can aggravate symptoms of dry eye and can be the difference between being comfortable or not. There is not necessarily any escape by heading indoors, as virtually all central heating and air conditioning systems also remove moisture from the indoor air. In commercial aircraft, the cabin air is pressurized but is also dehumidified, so I encourage the use of artificial tears as often as every 30 – 45 minutes while in flight (if not asleep).

Moving air and air turbulence are also significant factors affecting eye comfort and wetting. Moving air and turbulence dramatically increase evaporative loss of the water portion of the tear film. Examples include using a hair dryer to style and blow-dry hair, or driving in a convertible with the top down in the desert. Even a slight amount of air movement can have a significant adverse effect upon eye comfort, and it sometimes affords great relief simply to adjust the fins on a vent directing air movement from central heating or air conditioning systems. The same holds true for A/C in a car, where there can be a trade-off between feeling that cool breeze on your face and maintaining good eye comfort. People reading this where the climate is colder should simply substitute “warm” for “cold” and “heating” for “A/C” in the above example.
While I do find it common for post-LASIK patients to have mild dry eye issues, these are typically easily treatable with some combination of the simple steps outlined here. It is with extreme rarity that I encounter any patient manifesting profound dryness or ocular surface disease.
The normal human tear film is about 98% water (with dissolved minerals or “salts” including sodium, potassium and calcium), about 1% lipid (an oily film that reduces evaporation, reduces tear breakup, and helps the lids glide smoothly over the corneal surface), and about 1% mucopolysaccharide (the “mucus” component, long water-soluble molecules that further stabilize the tear film, and promote adherence to the corneal epithelium). The watery portion of human tears are created by a combination of the tear gland and special mucin-secreting cells on the ocular surface.
Maintaining good hygiene, and good hydration, are essential to keeping the eyes comfortable. I recommend that people keep at least six factors in mind to accomplish this:
- Drinking adequate water or fluids;
- Use of Artificial Tears every ~2 hours or so during the day, for the first 10 – 12 weeks after LASIK; and thereafter as desired to maintain comfort;
- Use of lubricant gels at night, or liquid-gel drops during the day, as appropriate.
- Use of a small area humidifier when appropriate. Humidifiers are widely available at pharmacies, linen and bath supply stores, Costco and other retail outlets. Many people already own one, as they are commonly recommended for people with allergy/hayfever symptoms, and as adjunct therapy for children with respiratory problems. They range in cost from about $25 to over $100, but very decent ones are typically around $50, which is about the same as the cost of three bottles of artificial tears. I advise putting the humidifier in the room where it will do the most good (bedroom, home office, etc.). Then, instead of dry air sucking moisture out of the eyes, moist air can actually keep the eye surface comfortable. A side benefit is that your skin will love the moisture, too! We recommend the ultrasonic humidifiers rather than evaporative or vaporizer types, which are noisier.
- Good lid hygiene is important to maintenance of a good lipid tear layer. This is where all the advice about blepharitis, lid scrubs, hot compresses lid hygiene and lid massage comes in. If the lipid component breaks down, no amount of artificial tears will solve the problem. We treat blepharitis when appropriate, and endorse the use of moisturizing creams and/or lotions for the eyelid skin in those people that desire to use these products. Commercially available products to help cleanse the skin around the eyelashes (and reduce the bacterial counts growing there) include OcuSoft eyelid cleansing pads and Steri-Lid eyelid cleanser may be very helpful.
- In some people, beneficial effects are achieved with Omega-3 fatty acid supplements. Several companies offer over-the-counter supplements with such oils and fatty acids including Thera-Tears Nutrition and others.
Factors that adversely impact tear production
- Diuretics, as these medications remove water from the system;
- Antihistamines, either topical (eye drop) or systemic can have a drying effect, as they reduce secretions; the tear gland after all is a secretory gland too.
- Alcohol, even when consumed in modest or small quantities, gets into the bloodstream and the tears. It reduces surface tension of the tear film, leading to significantly increased evaporation.
- Cigarette smoking. The particulate nature of cigarette smoke can be directly irritating to the eyes, and the chemicals that are inhaled can adversely affect both ocular surface blood flow, tear secretion, and tear quality.
- Sedatives, sleep aids, or muscle relaxants. These all can decrease muscle tension, and can lead to incomplete closure of the eyes during sleep. If the eyes open even a little, evaporative tear loss can create significant dry-eye symptoms most notable upon arising in the morning.
- Cologne, perfume, fragrance, or after-shave. All these substances are bottled in liquid containing — you guessed it — alcohol, so each spray or splash is basically giving the eyes a large, direct dose of the alcohol, which increases tear loss though evaporation.
- Air travel. On commercial and private aircraft, cabin air is very dry, as the air is both dehumidified and cooled. If travelling by air within 3 months of LASIK, it is advisable to use artificial tears as often as every half hour while the plane is in flight (unless your eyes are closed as in sleep).
- “Get the red out” drops (Visine, Naphcon-A, Opcon-A and others). The fluid in Visine contains polyvinyl alcohol, which exerts a drying effect (see alcohol, above). When the effect of the constrictor drops wears off, there can be rebound leading to more congestion, more perceived need to use more drops, etc.;
- Acutane and certain other medications. Acutane adversely affects oil production by the eyelid meibomian glands, and is actually a known contraindication to LASIK per the FDA guidelines.
- Blink frequency and disruption of normal blinking. People that become intensely focused on work, particularly using computers, often blink with decreased frequency. This can lead to drying of the eye surface. The same factors hold true for people with certain hyper-thyroid conditions.
- Exposure to hot, dry air, particularly if blowing, or wind-related. Common when styling and blow-drying hair and other common situations.
- Exposure to drafts, breezes, or moving air from central heating or A/C systems. Often simply adjusting the fins on the duct openings to steer the moving air away from one’s face can afford dramatic reduction in discomfort;
- Exposure to aerosol chemicals or sprays that can be toxic or irritating;
Optimizing the ocular surface
- Artificial tears (preferably preservative-free or vanishing preservative) throughout the day. It’s almost impossible to over-use tears; some people insert as frequently as every hour or more. We prefer the “vanishing-preservative” formulations found in TheraTears and GenTeal drops. Unlike the twist-off tubes of preservative-free tears, which can’t be re-closed and therefore don’t travel well, the vanishing preservative products come in a large bottle with a screw-cap and can be carried in a pocket, purse or backpack.
- Gel lubricant at night, with or without liquid-gel lubricant during the day, to supplement the effect of artificial tear drops.
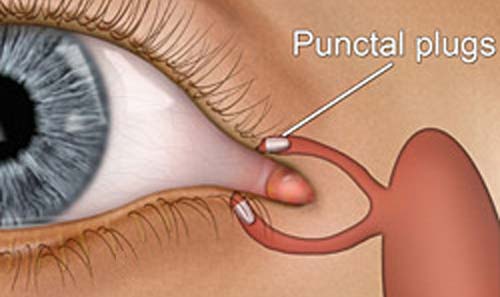
- Collagen Punctal Plugs . Normally, tears from the eye drain through a tiny channel to the nasal passages. The openings from the eyelid edge into the tear duct (there are normally two in each eye, near the nasal corner of each upper and lower lid) are called the puncta. Placing either a temporary (collagen) or permanent (silicone) plug in the punctum can reduce the rate of drainage of tears from the eye surface. At LA Sight we place the temporary (collagen) plugs with some frequency but use the more permanent (silicone) plugs only very rarely, and only in the lower lid puncta. I have almost never found it necessary to place plugs in both the lower and upper lid puncta.

Silicone punctal plugs have a ‘champagne cork’ design and do not dissolve, so they can last for years. However, in rare instances they can cause certain side effects and trigger a scar-tissue reaction around them (similar to fibrous capsule formation around silicone gel breast implants). For these reasons, we only use silicone plugs very rarely.
Use of a humidifier on the night-stand in the bedroom, to increase humidity around your face and eyes overnight.
Blepharitis treatment as necessary
Specially-formulated drops such as Fresk-Kote contain medication that can stabilize and soothe the irritated ocular surface, and speed healing of ocular surface discomfort.
- Restasis and other prescription medications when necessary. These can be used in treatment of severe dry eye and ocular surface disease.
- Preparation of special autologous serum-containing tears . Some experts feel that the addition of serum proteins to preservative-free tears affords a natural and supportive environment to the tear film, which can restore comfort. Serum is a component of human blood (the fluid remaining after clotting factors and blood cells are removed) so requires blood drawing and preparation by a medical professional. We have found this to be of value after PRK surgery in rare cases but have not employed this to treat dry eye save for very exceptional cases.
Helping the eyes maintain their moisture helps in so many ways. Think of your eyes like orchids, which thrive in moist, warm climate; and you will appreciate how simple, and important it is to keep them moist to keep them happy!
The above is an extensive but incomplete list of factors that can cause “dry eye”, and a review of suggested remedies. It is our goal that patients achieve excellent vision and optimum eye comfort. Using the above as a guide and reference, we personalize our recommendations to the needs of each patient. With diligence on everyone’s part, we are able to treat those patients who are uncomfortable, unhappy, or functionally impaired due to ocular surface symptoms including dry eye.